Shop By Category
Browse our selection of medical equipment and supplies

We Offer a Wide Range or Rental Equipment
Welcome to MedEquip Shop, your trusted destination for top-quality medical supplies in Houston, Texas. Situated as a leading medical supply store at the core of Houston, we take immense pride in presenting an extensive array of products tailored to meet the varied requirements of our esteemed customers. Whether you are a healthcare professional, caregiver, or an individual seeking medical supplies, we are dedicated to delivering the utmost quality in both products and services.
Tips & Helpful Resources
We are always here to help with maintenance tips and answer any questions. The tips, advice, and information you need to manage your health.
Your Complete Guide to Choosing the Best Medical Supply Store Near You
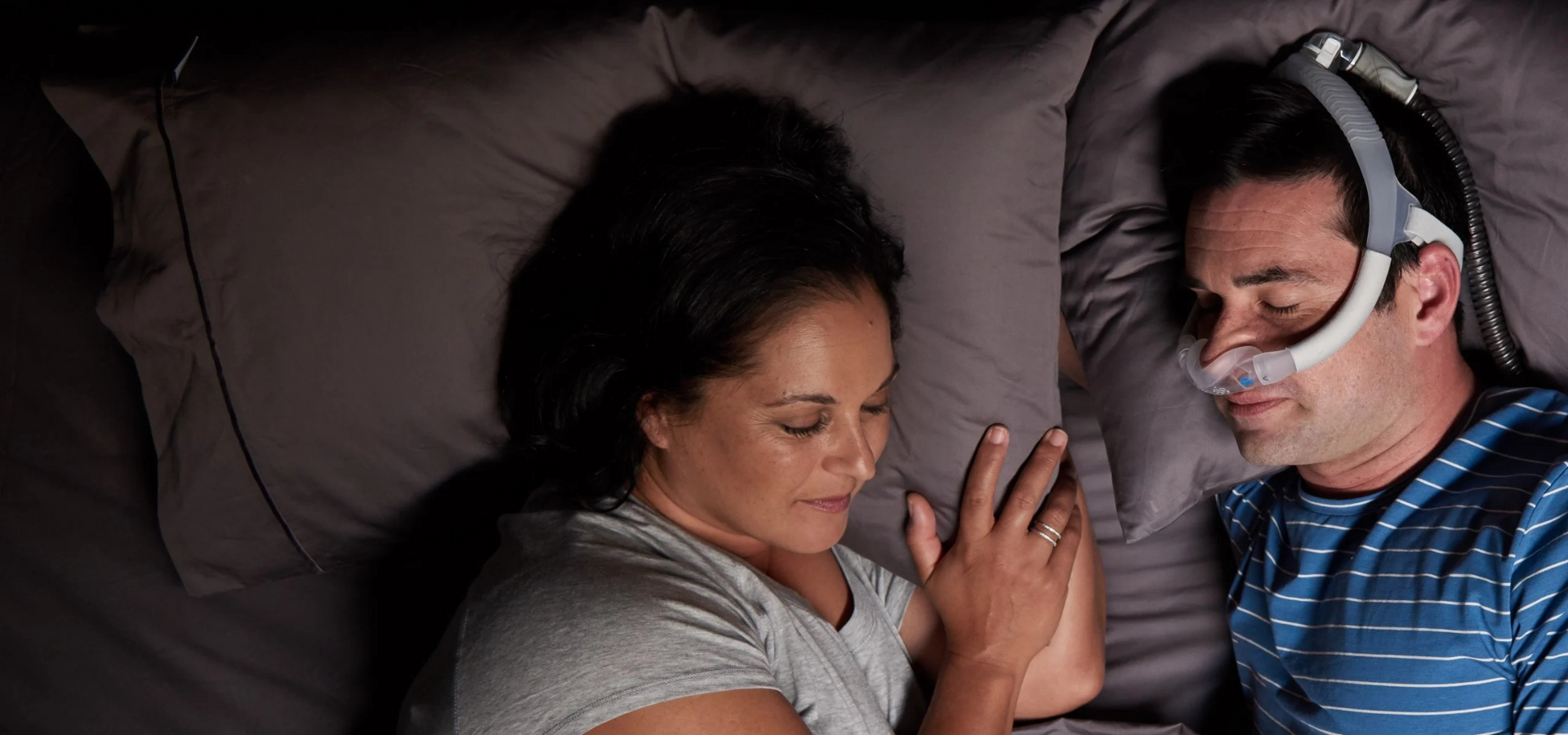
Finding the right medical supply store near me can make all the difference in recovery and home care. From medical equipment rental near me—like hospital beds, CPAP machines, scooters, and oxygen concentrators—to everyday home medical supplies near me, MedEquip Shop provides trusted solutions. This guide explores what to expect from a medical supplies store near me, why rentals are often the smart choice, and how to choose the best medical equipment store near me for your needs.
Read moreResMed AirFit N30i Mask: The Ultimate Guide to Comfort, Cleaning, and Replacement
The ResMed AirFit N30i Mask offers a lightweight, minimal-contact design with top-of-the-head tubing for greater comfort and mobility during CPAP therapy. In this guide, we explore its key features, proper cleaning routines, and recommended replacement schedules for CPAP supplies. Whether you’re searching for a “CPAP store near me” or shopping online for reliable CPAP supplies, the AirFit N30i is a top choice for effective and comfortable sleep apnea treatment.
Read moreTypes of Hospital Beds for Home Use | MedEquip Shop
What Types of Hospital Beds Are Available for Home Use? (The Complete Guide) Introduction: Why Choosing the Right Hospital Bed Matters When a loved one needs a hospital bed at home, families often feel overwhelmed by the choices. You’ll hear terms like manual hospital bed, semi-electric, fully electric, bariatric, hi-low, and even luxury home care beds. The question we hear most often is: “What types of hospital beds are available—and which one should I choose?” At MedEquip Shop, we specialize in cash-pay hospital beds and medical equipment. That means we don’t just hand you the one or two models your insurance approves. We help you understand the full spectrum of options so you can make the decision that’s best for your family. This article is a complete guide to the different types of hospital beds available for home use. We’ll cover: Manual hospital beds Semi-electric hospital beds Fully electric hospital beds Hi-low hospital beds Bariatric hospital beds Trendelenburg & specialty hospital beds Luxury home care beds We’ll also discuss mattresses, accessories, and the honest pros and cons of each option. Manual Hospital Beds What They Are Manual beds are the simplest and least expensive. They use hand cranks to adjust the head, foot, or height. Pros Lowest upfront cost ($900–$1,500) No electricity required (can be adjusted even during power outages) Durable—fewer moving parts to break Cons Caregivers must do the lifting (cranking is tiring, especially for frequent adjustments) Patients cannot adjust themselves independently Limited comfort for long-term care Who They Work For Best for short-term recovery where budget is a concern and caregiver support is strong. Browse our selection of affordable hospital beds. Semi-Electric Hospital Beds What They Are Semi-electric beds combine electric motors for the head and foot adjustments with a manual crank for height adjustment. Pros Easier for patients to adjust themselves Caregivers don’t need to manually raise/lower head or foot sections Affordable ($1,200–$2,000) Cons Bed height still requires manual cranking Not as convenient as fully electric models Who They Work For Great for patients who need regular position changes but don’t require frequent height adjustments. Fully Electric Hospital Beds What They Are Fully electric hospital beds allow head, foot, and height adjustments by remote control. Pros Maximum independence for patients Easier for caregivers—no manual cranking Improves safety during transfers Available in many designs and upgrades Cons More expensive ($1,800–$4,500) Requires electricity (backup battery optional in some models) Who They Work For The most popular option for families choosing cash pay. Ideal for long-term care, elderly patients, or anyone needing frequent adjustments. Shop our fully electric hospital beds. Hi-Low Hospital Beds What They Are Hi-low hospital beds can be adjusted from very low (7–9 inches off the ground) to standard height. Pros Excellent for patients at risk of falling (dementia, Alzheimer’s) Safer for transfers when raised higher Fully electric operation Cons Higher cost ($2,500–$5,000) Larger frames require professional setup Who They Work For Patients with high fall risk or advanced care needs. Bariatric Hospital Beds What They Are Bariatric hospital beds are built with wider frames and stronger motors, supporting 500–1,000+ lbs. Pros Wider sleep surface (42”, 48”, or 54” options) Extra durability for heavier patients Fully electric operation Cons Expensive ($3,000–$7,000+) Require more space in the room Delivery may require multiple technicians Who They Work For Patients who need extra strength and width for comfort and safety. Explore our bariatric hospital beds. Trendelenburg & Specialty Beds What They Are Some hospital beds offer advanced features like Trendelenburg positioning (tilting the entire body), reverse Trendelenburg, or lateral rotation beds for complex care needs. Pros Essential for spinal injuries, respiratory conditions, and advanced wound care Improve circulation and comfort for immobile patients Cons Very expensive ($5,000–$10,000+) Typically not covered by insurance Require larger spaces and strong electrical supply Who They Work For Patients with complex medical needs requiring specialized positioning and pressure relief. Luxury Home Care Beds What They Are Luxury hospital beds combine medical functionality with high-end home furniture design. They often feature wood trim, upholstered headboards, and concealed motors. Pros Look like regular home furniture Provide comfort and dignity for patients Fully electric with premium mattresses Cons Premium pricing ($4,000–$10,000+) Usually not covered by insurance Who They Work For Families who want a bed that blends into the home environment while still offering full hospital functionality. See our luxury-style hospital beds. Mattresses for Hospital Beds A hospital bed is only as comfortable as the mattress it supports. Options include: Innerspring mattresses – Basic, lowest cost. Foam mattresses – More comfort, pressure relief. Alternating pressure/low air loss mattresses – Prevent bedsores, improve circulation. Bariatric mattresses – Wider and stronger for heavier patients. Explore our hospital bed mattresses. Essential Accessories Accessories make caregiving easier and safer: Overbed tables – Meals, reading, laptop use. Patient lifts – Safe transfers from bed to chair. Side rails – Half rails, full rails, or assist bars. Trapeze bars – Help patients reposition independently. Bedside commodes – Convenient for nighttime use. Honest Observations From Families Because we sell cash-pay beds, we hear real stories every day: Families almost always prefer fully electric over manual or semi-electric. Hi-low beds are increasingly popular for fall prevention. Aesthetics matter—many families choose luxury beds for living rooms or master bedrooms. Insurance customers often regret not going cash pay after seeing their limited options. Real-World Scenarios Scenario 1: Short-Term Recovery A patient recovering from knee replacement chooses a semi-electric bed for 2 months. Affordable, returned after use. Scenario 2: Long-Term ALS Care A family purchased a hi-low bed with an alternating pressure mattress. It prevented sores and made caregiving safer. Scenario 3: Dignity in Living Room Care A family caring for their mother in the living room invested in a luxury-style hospital bed. Visitors saw a beautiful bed, not a medical device. Conclusion: Choosing the Right Hospital Bed So, what types of hospital beds are available for home use? From manual beds to luxury models, families today have more choices than ever. If you go through insurance, you’ll be limited to basic manual or semi-electric models. If you choose cash pay, you can select from the full range: fully electric, hi-low, bariatric, specialty, or luxury designs. At MedEquip Shop, we believe in transparency: the right bed is the one that balances comfort, safety, and dignity for both patient and caregiver. Explore our full hospital bed collection today to find the model that fits your home and your loved one’s needs. Related Questions What’s the difference between manual and electric hospital beds? What type of hospital bed is best for long-term care? What’s the best hospital bed for fall prevention? How wide is a bariatric hospital bed? Do hospital beds look like normal beds?
Read more
Reliable Medical Equipment for Every Need
Explore our wide range of durable, FDA-compliant medical equipment designed to support patient care in homes, clinics, and hospitals. Quality you can trust. Service you can count on.
Need Assistance or have questions?
Give us a call. Our trained staff are available and ready to help!